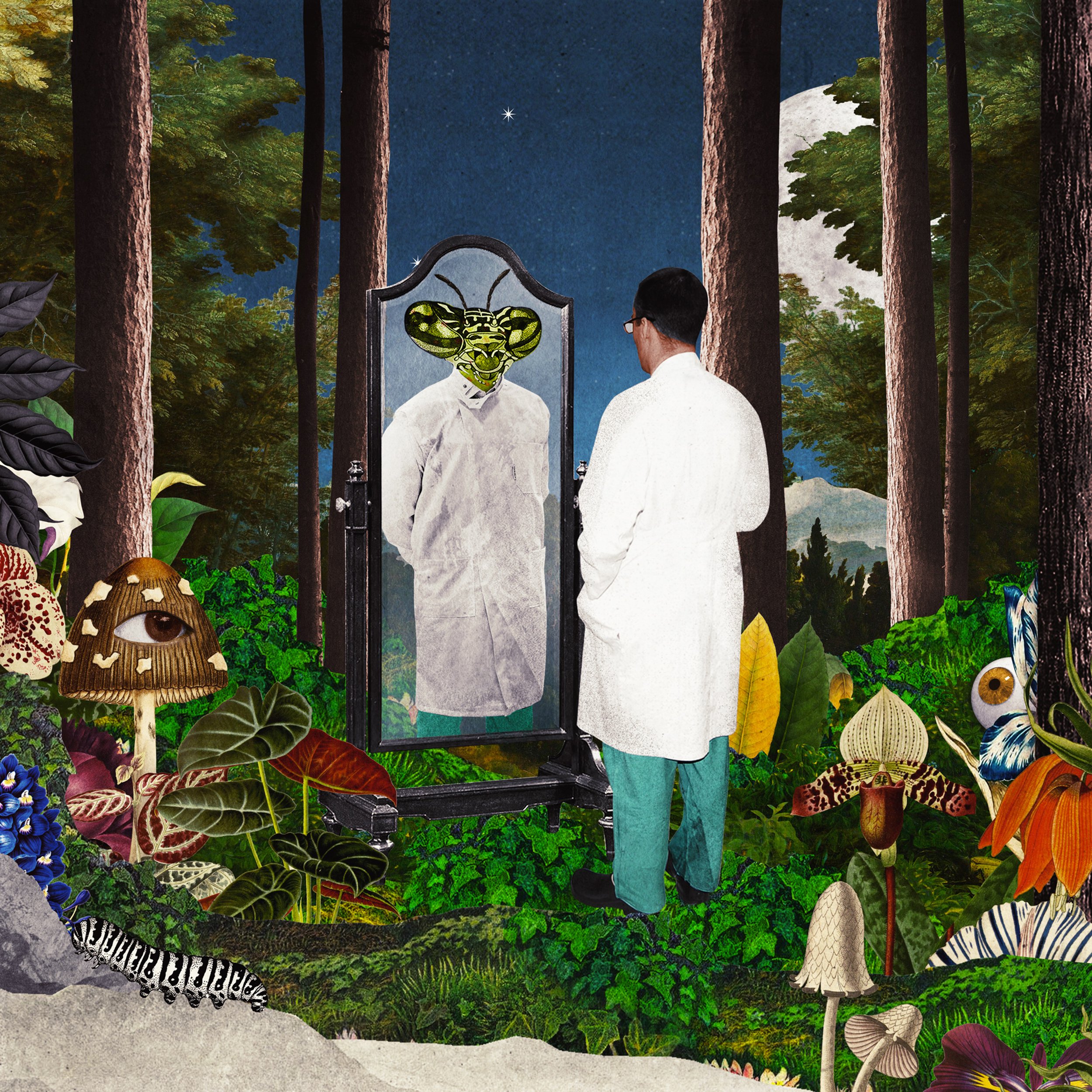
2. The Ideal Doctor
Episode Synopsis
Medical culture is filled with impossible ideals: the resident expected to work a 28-hour shift without complaint or error; the surgeon with the steel bladder; the doctor with perfect bedside manner; the student with all the answers. How should a doctor look, act, think, speak, dress, feel? What should they value? In this episode, we explore the concept of “The Ideal Doctor.” Where do these “ideals” come from? How are they communicated? And what do they have to do with shame?
Behind The Scenes
In this episode, we wanted to explore the difference between the “ideal self” and the “actual self,” as well as the internal and external sources of those ideals. To start, we did some research into the origins of the concept of the “ideal doctor” and stumbled upon an old Hippocratic text entitled “The Ideal Physician.”* Despite being written 2,000 years ago, we were shocked by how familiar it sounded. Deciding which stories to include in this episode was tough, as there were so many to choose from. In the end, we chose to go with a mixture of stories related to endurance, identity, and more.
* The collection of works known as the "Hippocratic Corpus" was written by a collection of physicians who lived around the time of Hippocrates. Hippocrates himself may have only written a handful of these writings.
CONTRIBUTORS
Adrian Anzaldua, MD
Shireen N. Heidari, MD
Margaret Leddy, PA-C
Charlie Varon
And other healthcare professionals who wish to remain anonymous
PRODUCTION TEAM
Host & Co-creator: Emily Silverman, MD
Co-creators & Research Leads: Luna Dolezal, PhD & Will Bynum, MD
Producer, Editor & Audio Engineer: Sam Osborn
Producer & Assistant Editor: Molly Rose-Williams
Additional Producing: Adelaide Papazoglou
Production Coordinator: Penelope Lusk
Medical Student Producers: Corinne April Iolanda Conn, MPH & Nikhil Rajapuram, MD
Impact Campaign Manager & Assistant Producer: Carly Besser
Executive Producer: Alison Block, MD
Chief Operating Officer: Rebecca Groves
Exeter Team Coordinator: Alice Waterson
Series Illustrator: Beppe Conti
Music: Blue Dot Sessions
SPONSORS
This episode of The Nocturnists is sponsored by #FirstRespondersFirst, a fund of the Entertainment Industry Foundation (EIF), a 501(c)(3) charitable organization.
Shame in Medicine: The Lost Forest is made possible in part by the Shame and Medicine project at the University of Exeter, funded by the Wellcome Trust.
The Nocturnists is supported by the California Medical Association, and people like you who have donated through our website and Patreon page.
-
Download the discussion guide for Episode 2, "The Ideal Doctor" here.
-
LISTEN:
Life After Medicine Podcast, “Are You Living Up to the "Healthcare Hero" Ideal? with Dr. Emily Silverman.
READ:
Dolezal L. Gibson M. Beyond a trauma-informed approach and towards shame-sensitive practice. Humanit Soc Sci Commun 9, 214 (2022).
Dolezal L. Rose A. and Cooper F. COVID-19, online shaming and health-care professionals. The Lancet. Vol 398. August 2021.
Hippocrates. The Physician. Workman B. K. They Saw It Happen In Classical Times. Oxford: Basil Blackwell, 1964. 64-65.
Miles S. Addressing shame: what role does shame play in the formation of a modern medical professional identity? BJPsych Bulletin. 2020.
Peters M. King J. Perfectionism in Doctors. BMJ Editorial. 2012.
WATCH:
Goldman B. Doctors make mistakes. Can we talk about that? TEDxToronto 2010.
Ofri D. Deconstructing our perception of perfection. TEDMED 2015.
-
The Nocturnists – Shame in Medicine: The Lost Forest
Ep. 2 The Ideal Doctor
Episode Transcript
Note: The Nocturnists is created primarily as a listening experience. The audio contains emotion, emphasis, and soundscapes that are not easily transcribed. We encourage you to listen to the episode if at all possible. Our transcripts are produced using both speech recognition software and human copy editors, and may not be 100% accurate. Thank you for consulting the audio before quoting in print.
Charlie Varon (as Hippocrates)
Hello, my name is Hippocrates of Kos. Yes, the Hippocrates. I've heard that these days I am referred to as "the father of modern medicine". I'm pleased to share with you a piece I wrote 2000 years ago titled, "The Ideal Physician":
“The position of a doctor must make him careful to keep his complexion and weight at their correct natural standard. For most people think that those who fail to take care of their own physical condition are not really fit to take care of that of others. Secondly, he must have a clean appearance, wear good clothes, using a sweet-smelling scent, which should be a totally unsuspicious perfume... Also he must observe rules about his non-physical effect, not only in being quiet but also in being self-controlled in all aspects of life... His character must be that of a gentleman, ... honorable and kindly towards all. For people dislike forwardness and interference,... He must also pay attention to his technical ability... In facial expression, he should be controlled but not grim. ...while a man who bursts into guffaws and is too cheerful, is considered vulgar.... He must be just in every social intercourse... Towards all these, therefore, he must keep himself under strict self-control. The above, then, are the physical, psychological requirements for a doctor.”
Emily Silverman
You're listening to The Nocturnists' Shame in Medicine: The Lost Forest. I'm Emily Silverman. In the last episode, we talked about how shame is often triggered by an event, which causes us to compare our current self with an ideal self. But that begs the question, whose ideal? The reality is, we're all swimming in a narrative of what an ideal doctor is. And I use the word "doctor", but, really, this applies to any type of healthcare worker, including nurses, NPs, PAs, and so forth.
Some of these narratives about the ideal doctor are explicit: the resident expected to work a 28-hour shift without complaint or error, the doctor with the perfect bedside manner, or the student with all the answers. And some of these narratives about the ideal doctor are unspoken, part of the hidden curriculum in medicine: How should a doctor look, act, think? What should they value? And then, of course, there's our own personal vision of our ideal self.
Today we'll be hearing stories from healthcare workers who are grappling with the concept of the "ideal doctor". We'll hear about ideals of endurance that are impossible to achieve, ideals related to self-expression and personality type, and ideals of altruism that collapse in the real world. Where do these ideals come from? Do they make us better doctors? And, if not, what do they do?
Shireen Heidari
When I was a resident, the unspoken rule was, that if you called out sick, you had better be completely unable to get to work. Some of us even would say, you know, only if you're dying. So, I remember the time where I finally had to call out sick. And it was the end of intern year. I was on call overnight. I was about three hours into my shift, so I had already admitted a few patients from the emergency room, checked on a few floor patients.
And I don't remember exactly how it started, but all of a sudden, I just knew that something wasn't right. And I started to feel contractions of my abdominal muscles; I started to taste this kind of bitter taste in my mouth. And before I knew it, I was running towards the trash can. When it seemed like there was nothing else left in my body, I got up. I took a deep breath, and I called my chief resident. And I said, "I'm so sorry, but I am actively vomiting, and I probably shouldn't be seeing patients." And, to her credit, my chief came in. She covered the rest of my shift, and basically said, "I'll see you in the morning. Just come to Rounds, so you can present the patients that you've already admitted."
I signed out the service, while lying flat on a cot, and slept; dragged myself to Rounds the next morning. I must have looked pretty horrible, because as I was telling the team about the patients I had admitted, the attending physician was writing a prescription for Zofran. And handed it to me, and called the pharmacy to make sure that I could fill it on my way out the door. And I get home, having filled the Zofran prescription, I collapse on my couch and I proceed to sleep for a day and a half. Some of my co-residents are dropping off soup, texting... trying to, you know, joking about how they heard I was dying of dysentery,... you know, but really checking in on me; because if you took more than two sick days, you had to make it up from your vacation, and you also had to pay back the days to the person who covered you. And it just was another reason why we didn't call out sick.
And so, by Thursday night, I'm starting to feel a little bit better. And I get a message that says I still need to come into clinic Friday morning, because it's the end of the year and I have to see two more patients to meet my numbers. And, to their credit, the person who sent me this message did not know how sick I was. So, I dragged myself to clinic. I walk in the door, and am immediately handed a mask by the clinic staff up front, at the front desk. And, I must look so horrible that multiple patients asked me if I should even be there. Meanwhile, unbeknownst to me, my other chief basically decides that I'm so sick that I need to be booked on to his clinic schedule. And when I finish seeing my patients, I basically get checked into an exam room myself. And ultimately, it is decided that I need IV fluids because I'm so dehydrated.
So, mind you, I've just seen several patients. But now, I am absolutely the patient. It takes two or three tries to get an IV into my arm. And I am sitting in my own clinic, getting a two-liter fluid bolus. And then suddenly, there's this flurry of activity, where doors start swinging shut. And one of my friends comes in, and goes: "Well, I'm sorry, but the new interns are here, and we're shutting all the doors, and I really don't think they should see you in your current state." And I just start laughing. Because essentially, in my head, I'm going "Oh my gosh, they're hiding me from the interns who are replacing us."
There I was, thinking this is what it took: that I worked myself to the point of needing to be rehydrated in my own continuity clinic. And it wasn't about the program. I would, you know... It wasn't really about anything other than this is what we were taught: that we should be superhuman and that even though we provided medical care, we wouldn't need it ourselves. And that couldn't have been further from the truth.
Joy
My name is Joy and I am a first-year internal medicine resident in Northern California. Over the years of being a university student on financial aid, then a research assistant, living in the most expensive city in the world, then a medical student in six-figure debt, I have acquired my own personal art collection. It lives in my nightstand in the form of a stack of inconsistently sized postcards, printed with my favorite artworks from museum gift shops.
There is always one postcard that sits on my desk for a month or two, before I go through my nightstand and choose another. Probably the most obscure of this collection, is a postcard of a painting, called "Self Portrait," by Georgette Chen, from the National Gallery of Singapore. In it, Chen is in three-quarter profile, and a muted earthy-brown palette, with brushstrokes straddling that line between fine and impressionistic. She gazes sideways at me: chin up, hair pinned, unflinching. More than the "Mona Lisa", or "Girl with a Pearl Earring", it is her look I most wish I understood.
I found myself reading an evaluation from the leader of my cardiology block during my second year of medical school in the rural Midwest. "Joy is very hard to read, could not tell if she is disinterested or already knew the material, or what was going on." He was the first in a string of handful of 40 to 50-somethings, mostly white, all male, attendings who gave me some variation of this feedback. And, for years, I felt puzzled and ashamed. I felt like there was something wrong, that I couldn't be that emotive, extroverted, readably enthusiastic student, which on the surface seemed like such a simple expectation.
When the latest variation of this comment happened during my second week of intern year, for the first time, I walked out, feeling more anger than shame. Why is it my job to be readable? If my superiors were truly interested in my thoughts, why not just ask me? What I have never explained, is that as someone who has spent over a decade navigating the streets of Singapore, to Nairobi, to the rural Midwest by myself, that as a young woman who is not white, that as someone who is not unfamiliar with the variations of sexual harassment and assault, it is beneficial for me in most settings to seem impenetrable.
And expecting this to fundamentally change and a learning or workplace does not just happen. I can no longer count how many times I have looked at Georgette Chen's "Self Portrait" over the last six years, and wondered what her hold is on me. This year, I finally realized that this picture is the first time I have seen in art history, a self-portrait of someone who looks like me. Not through someone else's gaze, but through her own. Sometimes she looks at ease, sometimes defiant, sometimes aloof, sometimes tired. But then I realize that is my own projection. She is all of these things.
Margaret Leddy
The story begins when I was a PA student. You don't know what you want to do when you're a PA student, so you have several rotations and you're gonna figure it out. And I went on an Internal Medicine rotation. And there was just a lot of talking, and I remember thinking, "Can we please stop talking? Can we just go do?" And then I got on Surgery, and Surgery – it was just fun. We got to do things and fix things, it just felt right. And so I have been in Surgery ever since. And looking back over my career, I truly recognize that Surgery, in my life, (when it was introduced to me), it's kind of like my drug. I have to be very, very careful with it, because it's something that I love, but it's also something that almost destroyed me.
So, when I started in Surgery, I started in Orthopedics, and I wanted more. And so I went into being just a first-assist in the operating room. Just all surgery, all the time. Still wanted more. And so I went into Cardio-thoracic Surgery, and that was I mean, amazing amount of information and learning. And it was beautiful to see the heart beating, and then work on it and, you know, fix it. And, you know, make things better and it was... It was 15-hour days and it was on-call every other weekend and it was "life or death" all the time. I remember one time I called my husband and said, "I will pick up the kids today," which was a rare event. And literally, as I was walking out of the ICU, a patient coded and I was pumping on the chest, and I had a nurse grab my phone out of my back scrubs pocket to call my husband, say "I can't pick up the kids; there's a code." I was completely unreliable; my family took second place to the patients and the care, because it was it was "life or death". It didn't seem like a choice as to whether I was home or not, it just ... The patients needed me.
Fast forward 13 years into my career, with me in the bathroom at work, in a stall, crying. Because it all came tumbling down when one of my daughters was diagnosed with ADHD and was failing school. And I didn't know how I was going to get her help, because I couldn't reliably be anywhere, at any point in time. And, my other daughter – not wanting to call me when I was at work, because even though she needed to be picked up and was feeling bad, because she thought I would yell at her, and not be able to get off work. And I just thought, I can't do this anymore. My children were afraid of me. My husband didn't want to be in the same room as me. My body was breaking down. I had just gotten diagnosed with yeast in my esophagus, for which the physician that performed the EGD said he had never seen in an immune-competent patient. My immune system was so taxed from all of the stress for so many years, I couldn't fight off a simple yeast infection in my esophagus.
So not only were my relationships in a rubbles, my health was deteriorating, and that didn't even have to deal with the demons in my brain. And I sat there in the bathroom, crying, for so many reasons, but I think the biggest reason was shame. Was that I looked around, and I saw people around me every single day, who were keeping it all together, who had significant others, and marriages, kids, life. And they just made it all happen. Like, magically. And they were keeping it together. And they were doing a great job at work, and a great job at home. And I... I wasn't doing either. And I was so ashamed to admit I couldn't do it anymore, that I had probably stayed too long, doing something that felt like it was an addiction to me.
The OR... When you're in the OR, you get to escape. You don't have to deal with the outside world. You are right there, just concentrating on what's right in front of you. I didn't have to think about my kids or my stress or my anything, it was just... you just concentrated on what was in front of you. And I had to admit to myself that it was a toxic relationship; admitting that I needed to stop. And it was the best thing I have ever done. I am four years into a different sub-specialty now, and my relationships are better, and my life is so beautiful; I could cry. And really this is a story, you know, surrounding my complete and utter burnout. But there's so much shame attached to it.
Anonymous
I've wanted to be a doctor for as long as I can remember, it's not a super original story for an Indian American child, but it is one that is authentic to me. My dad is a physician. He's a Hematologist-oncologist, and he is the small-town doctor that is actually the backbone, I feel like, of a lot of our American healthcare system, but not really the stories that you get to hear very much on a day-to-day basis. My dad developed these really beautiful relationships with his patients. And so, whenever we were walking in the mall or in the airport, people would easily identify us, ask us if we were Dr. ....'s kids. And, just be like, "Oh my gosh, your dad saved my life." And our house was just full of all these gifts from his patients, like they would bring him venison, even though we don't eat red meat, like all these things that were such expressions of their gratitude.
I think the ideal doctor for me growing up was this person who was super-selfless, who had these, like, really beautiful and intimate longitudinal relationships with families, and who found all these ways to be, like, really present and involved in families' lives. It was something that you could do as your job, and then come home and live a life, and that those things could be really separate. And as I went through training, I was, like, oh, I think the messaging I'm receiving about what an ideal doctor is, is someone who's really efficient. And, like, someone who is able to, like, speak with families as succinctly and quickly as possible, and who has, like, a very multi-faceted identity, where clinical practice is part of it; advancing the field isa big part of your identity. And, who also, simultaneously, didn't have boundaries. In this version of the ideal doctor, they're, like, there's no time and space for accepting how things impact us.
Yeah, I remember this experience in my third year where, I think it was on my psychiatry rotation, and we had a, a woman who was navigating domestic violence and substance use. And something happened where somehow the perpetrator found out that he was being accused, and he called the medical team. And he was, like, "Why are people accusing me? She's lying. This is not happening. This is a lie." I was so distressed. I was, like, Oh, my gosh, like, this person is not going to be safe. I don't know how they're going to go home. I don't know what's going to happen to them. And I remember, at that time, feeling like, “Am I the crazy one here?” Like, is this.... and every time I brought that up, where I was, like, “Hey, like, maybe we should debrief the patient that died.... or the five patients that died this past month...” They'd be, like, “I don't think we have time to add that to, like, the schedule. Like, there's just no time for that.” And I think it just felt like this ideal doctor was someone who was so busy, who had so many things going on, but didn't have time for the right things. And I was like, “Oh, no. I have a really different relationship to this than I thought I was going to have. And I don't know if I should be here.
For so much of the training, a lot of the shame for me felt like I was so much more emotionally affected by what I was witnessing than other people. And I felt really ashamed. Like, I intellectually knew that empathy was good and that I had a lot of compassion. But the practicalities of it were that I would come home and be so sad, or I would come home... It was impossible for me to, like, not think about the things that had happened. So I feel like every month, I felt like I was re-committing to doing it.
I had an opportunity to walk in a park on a random spring day with a mentor of mine, who is one of the doctors I really admire. I remember it was a beautiful day. And it was probably one the few times that we had, like, met up outside of the hospital. And we essentially just, like, walked in a circle, like, around this big park for an hour, and she was, just like, yeah, like, “how do you think things are going?” And I think I probably had a lot of, like, ambitions of, like, what I was going to say, and, like, how, like, calm and collected I was gonna come across. And instead I was, like, “honestly, like, I'm so stressed. Like, before, every chance... I'm, like, I don't know, like, I'm like, what if those patients should have a different doctor?” We stopped, and she looked at me and said, "You know, nobody is a perfect doctor. But you are good enough."
And I remember hearing that. And her, just like, being so willing to normalize how much everyone is still learning, and how hard our jobs can be, and how hard it is to be a new attending. That was the first time that someone gave me permission to feel like I didn't have to do everything. And that, in fact, to believe that I could do everything was, in itself, foolish. Like, that... that wasn't... that was never going to be the right goal. And I think from that moment, I started thinking about: okay, if I am good enough to be here, and the problem is not whether I'm skilled enough or competent enough, maybe the question I should be asking myself is, like, who do I actually want to be when I'm there?
Maybe this is the part that people can totally disagree with me, but I think an ideal doctor is someone who doesn't learn just medicine, but who who learns about how to communicate, who learns about relationship, who learns about all the reasons why certain structural inequities exist in healthcare. Because all those things impact our patients just as much as the doses of the medications that we give, of the surgeries that we operate, like, those things are so deeply intertwined. And I think an ideal doctor carries a lot of hats, but ultimately, is also committed to thinking about their own well-being, and knowing that tending to their own well-being is how we can advocate for justice for our patients.
Adrian Anzaldua
So, this is at the end of my third year, on the surgery rotation. I was exhausted; I was burnt out. I was tired of getting up at four o'clock in the morning. I really needed a break. And I just thought: if I can just put my head down for two months and do this, I will be done with third year. And so, you know, as often happens, the first couple of days, you know, you're going through orientation, and they say "Alright, go to the resident room". A little, sweaty, windowless room: It's a mix of, like, an office space and a frat house. And then, inevitably, in all in all of these rooms, there's a stack of books that students or interns have left that, you know, are guidebooks: how to be a great surgery intern; how to be a great surgery clerk. I thought, "Oh, okay, well, I'm just sitting here."
So, I picked up this really famous book for third-year medical students in their surgery rotation, called Surgical Recall. And I'm flipping through and I get to page four, just right at the beginning, and I see this list, titled "The Perfect Surgery Student". I'm going through, and this is just a selection of some of the qualities that "the perfect surgery student" is supposed to have. A perfect surgery student never whines, never pimps his residents or fellow students or attendings, never complains. Is never hungry, thirsty or tired, is always enthusiastic, never makes a fellow student look bad, is never late; is always clean, smiles a lot and has a good sense of humor, makes things happen, isn't a know-it-all, loves the OR, never wants to leave the hospital, takes correction/direction/instruction very well...
Charlie Varon (as Hippocrates)
"He must have a clean appearance, using a sweet-smelling scent..."
Adrian Anzaldua
...is the first one to arrive at clinic and the last one to leave...
Charlie Varon (as Hippocrates)
"Also, he must observe rules about his non-physical effect, not only in being quiet also and being self-controlled in all aspects of life..."
Adrian Anzaldua
... is confident but not cocky, has a "can do" attitude and can figure things out on his own...
Charlie Varon (as Hippocrates)
"His character must be that of a gentleman,..., honorable and kindly..."
Adrian Anzaldua
...follows the chain of command, praises others...
Charlie Varon (as Hippocrates)
"... people dislike forwardness and interference, even if these... He must also pay attention to his technical ability..."
Adrian Anzaldua
...runs for materials, lab values, test results etc. before Rounds...
Charlie Varon (as Hippocrates)
"In facial expression, he should be controlled but not grim."
Adrian Anzaldua
...has a steel bladder and a cast-iron stomach and a heart of gold...
Charlie Varon (as Hippocrates)
"He must be just in every social intercourse..."
Adrian Anzaldua
...an individual who places his head to the ground and hammers through any and all obstacles to get a job done and then asks for more work; one who desires work...
Charlie Varon (as Hippocrates)
"The above, then, are the physical, psychological requirements for a doctor."
Adrian Anzaldua
Now I'm not this person. I've never been this person. And I think in this moment, I am going to have to hide myself. I am going to have to become someone that I am not, if this is what the standard is. And that's... that, to me, is shame. When you are asked to put yourself away, to hide yourself, because who you are, naturally, is something that... that the environment around you does not value. You shouldn't have to give up your identity and give up who you are in order to practice.
Emily Silverman
Thanks for listening to Shame in Medicine: The Lost Forest. To contribute your reactions and reflections to our shame series and to access additional resources like transcripts, discussion guides and more, please visit our website at thenocturnists-shame.org.
Next week's episode is called “Golden Ticket.” And it's all about how our lives before medical school – sometimes dating back to early childhood – can affect the shame experiences that come up for us in the professional workplace. See you next week.
Shame in Medicine: The Lost Forest was co-created by me, Emily Silverman, as well as Will Bynum and Luna Dolezal. Our producers are Sam Osborn and Molly Rose-Williams, with additional producing by Adelaide Papazoglou. Sam also edited and mixed the series. Thanks to Medical student producers: Corinne April Iolanda Conn and Nikhil Rajapuram. Production Coordinator: Penelope Lusk. Impact campaign manager and Assistant Producer: Carly Besser, and Exeter team coordinator Alice Waterson. The Nocturnists Executive Producer is Ali Block, and our Chief Operating Officer is Rebecca Groves.
The series illustrations are by Beppe Conti, and the music comes from Blue Dot sessions. Shame in Medicine: The Lost Forest was made possible in part by the Wellcome Trust and the Shame in Medicine project at the University of Exeter.
The Nocturnists is supported by the California Medical Association, a physician-led organization that works tirelessly to make sure that the doctor-patient relationship remains at the center of medicine. To learn more about the CMA, visit cmadocs.org.
Our show is also made possible with donations from listeners like you. Thank you so much for supporting our work in storytelling. If you enjoy the show, please follow us on your favorite podcast app so you don't miss an episode. While you're in there, you can help others find us, by leaving us a rating and review. To contribute your voice to an upcoming project or to support our work with a donation, visit our website at thenocturnists.com.
I'm your host, Emily Silverman.
See you next week.